Veteran Pain Management Programme
Dear Veteran,
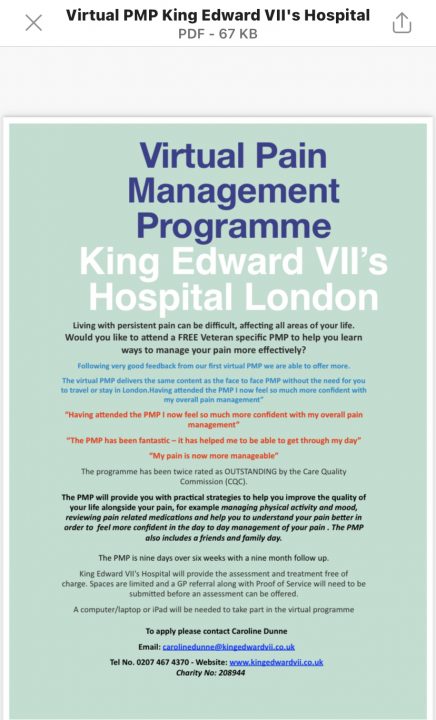
We are delighted to provide you with some information about the Pain Management Programmes (PMP) that areoffered to veterans at The King Edward VII’s Hospital in London.
A PMP is aimed to help people with persistent ongoing pain to improve the quality of their lives, the overall aims are toprovide you with practical strategies to help you improve the quality of your life alongside your pain, for example managing physical activity and mood, reviewing pain related medications and helping you understand pain better in order to feel more confident in the day to day management of your pain. Individuals with persistent pain can often feel isolated and unsure of how to plan for the future. Addressing these issues and others, PMPs are widely recognised as the treatment of choice for individuals suffering with persistent pain. Programmes not only offer a wide range of pain management strategies but also provide an environment for people to share their experiences and gain support from other group members.
The clinical team consists of a specialist physiotherapist, psychologist and nurse as well as medical consultants in pain medicine and psychiatry, all of whom work in the management of persistant/chronic pain. There are also non-clinical staff key to the service. They so far
have delivered 25 PMPs to vetereans over the past 6 years.
Due to the recent Covid 19 pandemic we have run the last 8 PMPs via tele confereing (Zoom) and this has proved successful. We will continue to run the future PMPs this way until we are advised it is medically safeto resume face to face group based programmes.
Assessment:
For you to gain the most from the programme, we will beinterested in knowing more about how the pain is affecting you and also what it is stopping you from doing, what you may like to do more of, return to or start doing. This information will form the basis for the PMP. Prior to a formal assessment you will be required to ask your GP to write to us supporting your possible invitation on the programme, you will sent a form to give them. Once the clinical team have this information you will be invited for an assessment with a multi-disciplinary team consisting of a Consultant in Pain Medicine, Specialist Physiotherapist, Consultant Psychiatrist and Consultant Psychologist, all who specialisein Pain Management. This assessment takes about twohours.
After the assessment you will then receive a letter telling you the next plan, much of which we will have discussed with you during the assessment. If we all think the programme will be of benefit you will be offered dates to attend. You will need to attend all the dates so it’s helpful to check diaries. We run regular programmes so it is always possible to attend a later programme.
Please note that the programme is not the best treatment option for everybody and not all patients with persistant pain find it helpful. If someone is experiencing multiple physical and psychological difficulties, we might suggest alternative treatment options, better suited for the individual.
Measures: Information about our questionnaires:
In order to make a full assessment of your pain problem we need as much information as possible about you and your pain. Some of this can be gained from the interdisciplinary assessment, but we also find it helpful for you to fill out questionnaires. They are standard and used all over the world. We are aware that some of these questions can seem intrusive and filling in endless forms is a tiresome process. Research indicates that this information is important if the correct decision about treatment is to be made. These are also important as they help us to measure the improvements made during treatment.
Please be assured that your answers are totally confidential. If you have difficulty with any of the questions just leave them blank – we can discuss them during your assessment. Thank you in advance for filling out the forms. The results may also be used anonymously in research and to evaluate the outcome of the pain management programme, again with written permission of the patient. This ensures we continue to develop the programmes to meet the needs of those attending.
You will need a computer with both audio and video functions in order to participate in the video conference/Zoom based group.
How long is the Pain Management Programme:
The PMP is 10 days long; nine days over six weeks followed by a follow up day nine months later. Your family and friends will be invited to a day which we hope will support you further in your pain management. Your attendance to all days is key and absence will significantly affect the gains you can make.
What to expect on a PMP:
King Edward VII’s hospital have in place an agreement with the Nightingale Hospital mental health nurses. They will be offering Specific support to some veterans with any mental health issues that are outside of the pain management programme, for example, making referrals, discussing any issues raised by the questionnaires.
Our colleagues are not going to offer mental health treatment, but they will assist with any mental health concerns and identifying any referral pathways that are appropriate.
Accommodation and travel:
Once the PMP runs face to face, all of your travel and accomadation costs will be covered by The Centre for Veterns’ Health.
Inclusion:
British military veterans suffering from persistent pain and motivated to actively engage in a group-based pain management programme.
Exclusion criteria:
The programme is not suitable for:
Post-Traumatic Stress Disorder:
Patients will be assessed for PTSD. Individuals with mild to moderate symptoms can be accommodated on the programme, however, the focus will be pain management and not the treatment of the PTSD symptoms. Ongoing referrals for individual management of PTSD can be made, but often need to go via the NHS.
Common themes or “frequently asked questions” often discussed on the Pain Management Programme:
“Why is my pain spreading?”
“I want to get to the bottom of this”
“What is it?”
“How can I find out what it is and who is the person who can achieve this?”
“I have been told it is all in my head”
“All I have been given is pills”
“The doctor never listened”
“How can it be that one doctor says this is this and the other one comes up with something completely contradictory?”
“I’ve had physiotherapy before, why more? Why is this any different? I really need more hands on”
“Surely – I need to just push through the pain?”
“How do I explain it to other people – they don’t understand”
Topics include:
Please find below the link to a scientific paper the clinical team have published:
Jannie Van Der Merwe*, Suzanne Brook, Claire Fear, Maxwell J. Benjamin, Gerald Libby, Amanda C. de C. Williams and Andrew P. Baranowski: Military veterans with and without post-traumatic stress disorder: results from a chronic pain management programme https://doi.org/10.1515/sjpain-2019-0182
If you have any queries or would like more information about the PMP please call Caroline Dunne 0207 467 4370 or email on carolinedunne@kingedwardvii.co.uk.